Our genetics play a larger role in our hormones than most people think. Obviously, diet, lifestyle, and environment are the primary dictating factors of hormonal harmony, but our genetic predispositions can cause those factors to tip the scales in our favor or to our detriment.
Hormones need to be produced, transported, properly utilized, and then metabolized (cleared or turned into another substance). There are a seemingly endless number of things that can affect each step, with stress and toxins being at the top of the list.
Types of Stress
Stress comes in many forms. The most commonly known and discussed ones are:
- Your everyday garden-variety emotional/mental stress of schedules, relationships, daily tasks,work, etc.
- Physical stressors like over-exercising or never exercising, physical injury, infections (viral, parasitic, bacterial), and chronic pain.
- There are also lifestyle/environmental stressors like pollution, smoking, less-than-optimal diet, heavy metals, and toxins from the plethora of modern day products we are constantly exposed to (new building materials, body care products, cleaning products, etc.).

All these forms of stressors cause oxidative stress. Oxidative stress happens when there are not enough antioxidants to neutralize the free radicals that are caused by stressors, and it leads to cell and tissue damage.
Detoxification
We need to be able to properly detoxify these stressors so they don’t derail our hormones! While we can’t literally detoxify mental/emotional stressors, we can manage them with things like yoga, meditation, mindful breathing techniques, and learning how to set healthy boundaries and say ‘no’ to things.
The liver and kidneys are key players in detoxifying the other forms of stressors. There is no way we can have hormonal harmony if the liver is overwhelmed or sluggish. The liver regulates and metabolizes many different hormones including thyroid hormones, sex hormones, and adrenal/stress hormones.
The body makes hormones and they travel to where they need to go. When they arrive, they fit into a cellular receptor, which is like a specific keyhole for each substance. Once the hormone activates the receptor, it signals the cell to do something. The “used” hormone then gets sent to the liver to be metabolized through phase 1 and phase 2 liver detoxification processes (more on the genetics of this ahead). It then gets sent on its way to the gut to get eliminated from the body.
When we have substances that affect or mimic our hormones, like xenoestrogens (“foreign estrogens” that come from things like plastics, receipt paper, pesticides, and ingredients in cosmetics and body care products), they fit into cellular receptors, but instead of signaling the cell to do something, it’s like putting super glue into the keyhole. The cell is not given a proper signal to do its thing, so the xenoestrogens cannot be properly metabolized. This causes a buildup of both the xenoestrogens, as well as the body’s own endogenously (made by the body) produced estrogens, leading to estrogen dominance which is so common these days.

If we can limit the amount of toxins that our lovely livers have to process, the liver will have more energy to do what it was designed to do, including metabolizing the hormones our bodies’ produce.
Genetic Influence on Hormones and Fertility
In addition to the genes that directly relate to hormones, the most important genetic variants that can affect hormones and fertility are genes dealing with antioxidant production, phase 1 (CYP genes), and phase 2 (methylation, glucuronidation, sulfonation, glutathione conjugation related genes) liver detoxification. However, there are quite a lot more genes that can affect your hormones, which is why getting a personalized reading of your genetic blueprint can give you so many answers!
Genes Related to Hormone Metabolism
Cytochrome P450 (CYP) – This gene makes enzymes that are involved with hormone synthesis and break down. CYPs metabolize thousands of chemicals that are made by the body (endogenous) as well as the chemicals we are exposed to through diet and environment (exogenous). Some CYPs metabolize multiple chemicals, while others only metabolize one specific chemical.
CYP1A1 – This gene is involved with the first step of metabolizing estrogen into the desirable 2-hydroxyestrone estrogen. CYP1A1 genetic variants cause an upregulation in enzymatic activity which may be protective against 4-hydroxyestrone estrogen. This pathway can be blocked due to genetic predispositions or environmental toxins.
CYP1B1 – This gene is responsible for the first step of metabolizing estrogen, but shuttles it down the undesirable, DNA-damaging pathway that makes 4-hydroxyestrone. 4-hydroxy estrogen is a potent estrogen that may be oxidized into carcinogenic compounds. CYP1B1 variants cause an upregulation in activity, increasing the production of potentially harmful metabolites (dubbing this pathway the “breast cancer pathway”) that increase oxidative stress and demand more of the body’s glutathione (the body’s ‘master antioxidant’), potentially depleting its levels. In the over 50,000 genomes in the interpretation software that I use, CYP1B1 variants are infrequently variated and are quite clinically significant even with a heterozygous variant (having a copy from one parent).
What this means is that it might not be a good idea for people with CYP1B1 variants to take a bunch of estrogen (birth control, fertility treatments, hormone replacement therapy) unless they are working with someone that will closely monitor their estrogen metabolites and work to encourage shifting them from the CYP1B1 pathway to the CYP1A1 pathway.
CYP19A1 – While most estrogen is made in the ovaries of cycling women, some estrogen is made from the conversion of testosterone with an enzyme called aromatase. The aromatase enzyme, encoded by the CYP19 gene, converts testosterone to estrogen. Variants in this gene cause an upregulation in aromatase activity, which is why having genetic variants in CYP19A1 has been associated with increased risk of endometriosis and estrogen sensitive cancers. This gene is also involved in the synthesis of cholesterol, which is the precursor to all our sex and stress hormones. It is important to note that many substances affect CYP19A1 activity like DDT, aflatoxin (produced from mold), and many phytonutrients.
CYP3A4 – In addition to playing a part in the metabolism of cortisol, estrogen, and testosterone, this enzyme metabolizes approximately half the drugs (and organophosphates) in use today.
Variants here will decrease the function of CYP3A4 activity.

CYP21A2 – This gene is responsible for converting progesterone to cortisol. Variants here can block this conversion and can cause low cortisol levels, but can also spare progesterone.
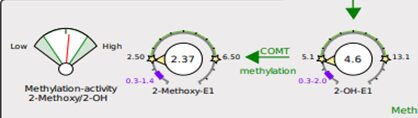
COMT – This gene, Catechol-0-Methyltransferase, is involved with metabolizing catecholamines (certain neurotransmitters) and the methylation of estrogens (via the phase 2 liver detox methylation pathway) to clear them from the body. Studies have shown association of COMT variants with PCOS, depression, preeclampsia, premature ovarian insufficiency, estrogen metabolism, endometriosis, and miscarriage. Having variants in your COMT gene can slow the metabolism of estrogens. SAMe and magnesium are cofactors for this enzyme to work.
Additional Less Commonly Discussed Genes
SHBG – The SHBG gene regulates the bioavailability of sex steroids by binding androgens, particularly testosterone and estrogens.
DIO1 – Deiodinase-1 gene. Involved with conversion of thyroid hormones T4 to T3 and their degradation. This enzyme is iodine and selenium dependent.
SULT1A1 – Just as estrogen needs to be methylated, it also needs to be sulfated, which takes place in the liver’s phase II detoxification pathway of sulfonation. Estrogen metabolism may be more strongly compromised (leading to estrogen dominance) when SULT variants occur in conjunction with other genetic variants involved with estrogen metabolism (COMT and CYP1B1).
The DUTCH test is a great way to see what is functionally happening with your hormone metabolism. This test looks at urinary metabolites, which are the hormones your body has used and is now getting rid of. This is a superior method of testing compared to measuring what’s in the blood, because we always want to be sure to look downstream, beyond just hormone production.
Knowing your genetic predispositions and how they may be expressing can give you accurate information to consider before utilizing any hormone therapies, whether that’s birth control, IVF, or hormone replacement therapy. Genetics tell you where the pathway may be going haywire and how to appropriately support it.
There are so many moving pieces that an automated analysis of your genetics won’t catch all the moving parts. This is where thoughtful human interpretation really makes an indisputable difference.
Interested in learning about your genetic profile?
Purchase your Functional Genomics Personalized Analysis & Interpretation
Purchase the 23andMe Raw Data Interpretation
View the webinar – Deep Dive: Understanding Genetics to Build your Personalized Road to Health
Buy the book – Enhancing Fertility through Functional Medicine: Using Nutrigenomics to Solve ‘Unexplained’ Infertility
Follow me @FunctionalFertilitySolutions (Instagram) for more info like this, and feel free to contact me at Info@JaclynDowns.com!